After finally finishing my checklist prior to starting chemo, it was time.
Chemo Day #1
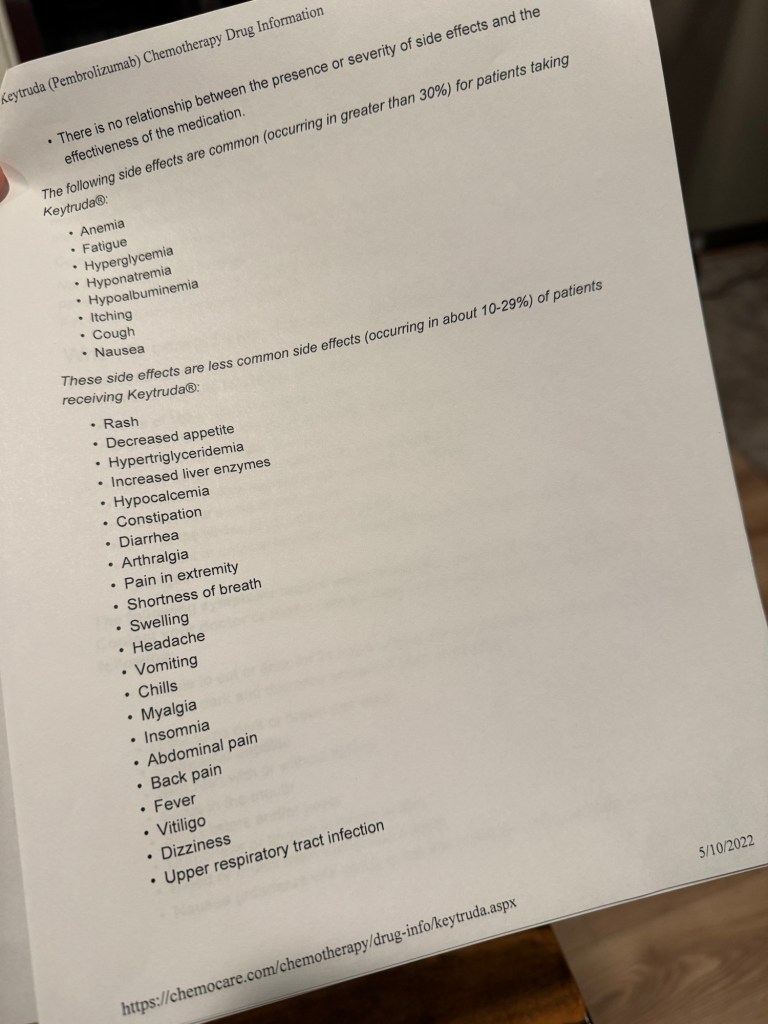
Every chemo session starts with a lab draw, doctor’s appointment, and scheduler visit. Then to the chemotherapy suite for infusion. It’s quite the ordeal, spending nearly 6-8 hours at Cancer Care Northwest (CCNW) depending on how backed up the doctor is that day. Some days we waited up to an hour just to see the doctor before starting the infusion. The doctor’s appointment consisted of reviewing my labs for the day, checking my weight, checking my vitals, and my signs/symptoms for the week. The first appointment was brief with a quick review of side effects to expect and things to look out for that ended with, “well let’s see how you do.”
When I say “we” I am referring to my husband and I. He came to every chemotherapy appointment with me, hung out or worked from his computer he brought with him. CCNW allowed 2 visitors during these infusions, so for my first infusion my friend of nearly 15 years joined as well, Brock. The first infusion was longer because they infuse at a slower rate to make sure I am tolerating it and I was also receiving Keytruda, an immunotherapy drug I was going to receive every 3rd treatment. So I found myself a chemo chair (one with a heated seat of course), set up my heated blanket my bosses got me and my new Stanley cup my friend Grace sent me. I got all situated and a couple nurses came up to me with a gift. They introduced themselves and said the gift was from Tracy (the RN that used to work at CCNW that helped me get my appointment with Dr. Moline at the start of all this). The gift consisted of a heat rice pack and a beanie. I remember the note, “A little something to keep you warm”. Which was very helpful, especially when I had to put on my cold mitts during the taxol infusion. The nurses were all very sweet and made me feel comfortable.
My nurse was Whitney. She explained everything very well, even when Brock asked her “what IS chemotherapy?” She was very short and blunt stating, “it is basically poison killing all of your fast growing cells”. SWEET.
The infusion starts with accessing your port (mine was left accessed due to having it placed the day before). Then you get your pre-meds (Benadryl, anti-nausea and Pepcid) which made me very drowsy and a bit woozy due to fasting and not having anything to eat. Then a 30 minute break before infusing chemo and Keytruda. I probably sat in the chemo chair for a total of 5 or 6 hours the first day.
We sat, talked, laughed and enjoyed each other’s company the entire time. Chemo #1 done. Now we wait and see what side effects I will get. . .