Undergoing an ovarian reserve test includes an ultrasound and blood draw. The ultrasound concludes how many follicles/eggs they can visibly see. This does not mean this is as many eggs as I have left. However, it gives them an idea of how many eggs can be retrieved. My ovarian reserve test came back sufficient enough to do an egg retrieval. They found 15 visible eggs. 15 egg lands in about 50th percentile for my age and my hormone levels came back at about 25th percentile for my age. The physician reports with these results the statistics show we should be able to retrieve between 9-11 eggs with an egg retrieval . With my first egg retrieval prior to chemotherapy, back when I was 28 years old, they retrieved 14 eggs. Out of the 14 eggs, 10 were mature enough to keep. Now, what are the next steps?
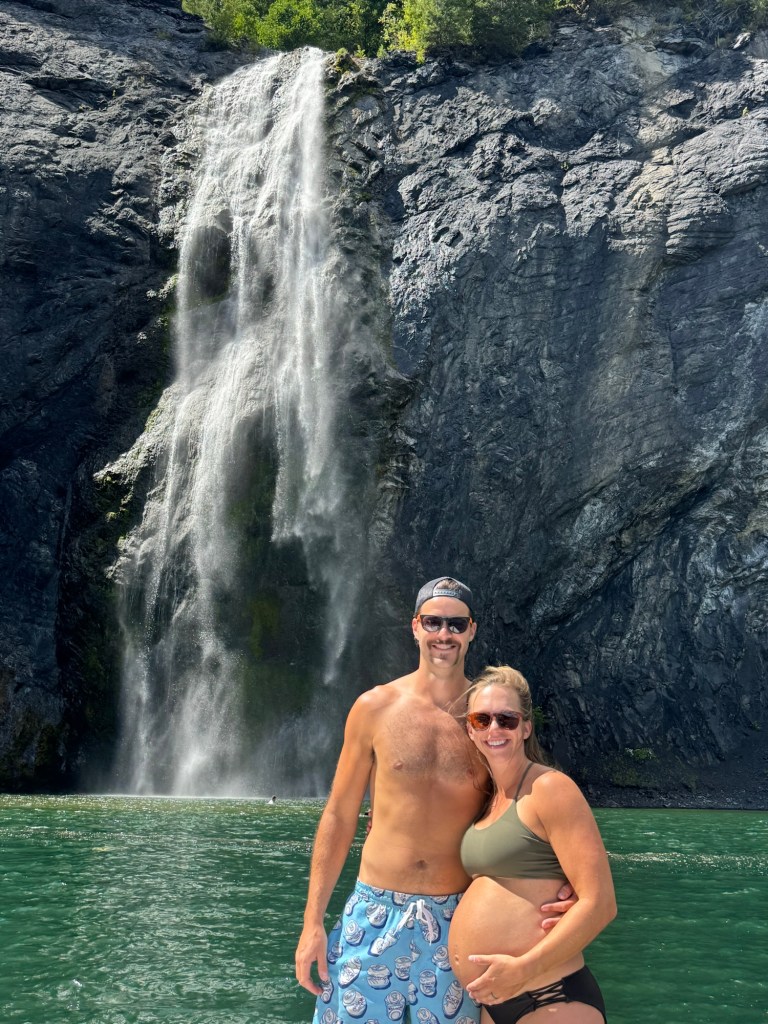
The start of an egg retrieval is based on your cycle. They await your next cycle and then have you begin birth control. Birth control is taken for about 2 weeks. You then stop birth control for about three days and begin the stimulation. The stimulation includes daily injections between 7 and 9 PM and 1 pill you take orally. You are to draw up, mix, and inject medication on your own each day to stimulate as many eggs for the egg retrieval as possible. These medications are ordered and delivered through a specialty pharmacy to your home and you are to watch a video on how to draw up an inject each medication. After my first injection all I can think of is “I did not miss this.” But I look at my daughter now who is about four months old, and think “but it was all worth it.” The injections and oral medication are taken for about four days and then you go in for an ultrasound and blood draw to assess your ovaries and hormone levels. They then reassess and adjust your medications if needed and you continue for another three days before going back in for an ultrasound and blood draw. You continue this cycle of ultrasound, blood draws, and medication adjustments until they feel that they have stimulated as many eggs as possible. As you get closer to the egg retrieval, they add an additional medication to inject in the morning between 7-9am. At this point, you are bloated, tired, crampy and your abdomen is bruised to the point where you are searching for a non-bruised place to inject medication. Once they feel you have stimulated as many eggs as possible, they prescribe a “trigger shot” that you inject exactly 36 hours prior the egg retrieval. You then have to take an ovulation test prior to 9am the morning after the trigger shot to make sure the medication absorbed. Exactly 36 hours after the trigger shot is when the egg retrieval is scheduled. They have you go in 45 minutes prior to the retrieval and meet with the physician and anesthesiologist.
The egg retrieval procedure is relatively quick (approximately 20 minutes) and involves the use of an ultrasound-guided needle to remove the eggs from the ovaries. The needle is inserted through the vaginal wall, and into each ovary, to draw out the eggs and surrounding fluid. The eggs flow through the needle into attached test tubes, which are then handed to the embryologist. “You will receive a call with the fertilization report the day following egg retrieval.”
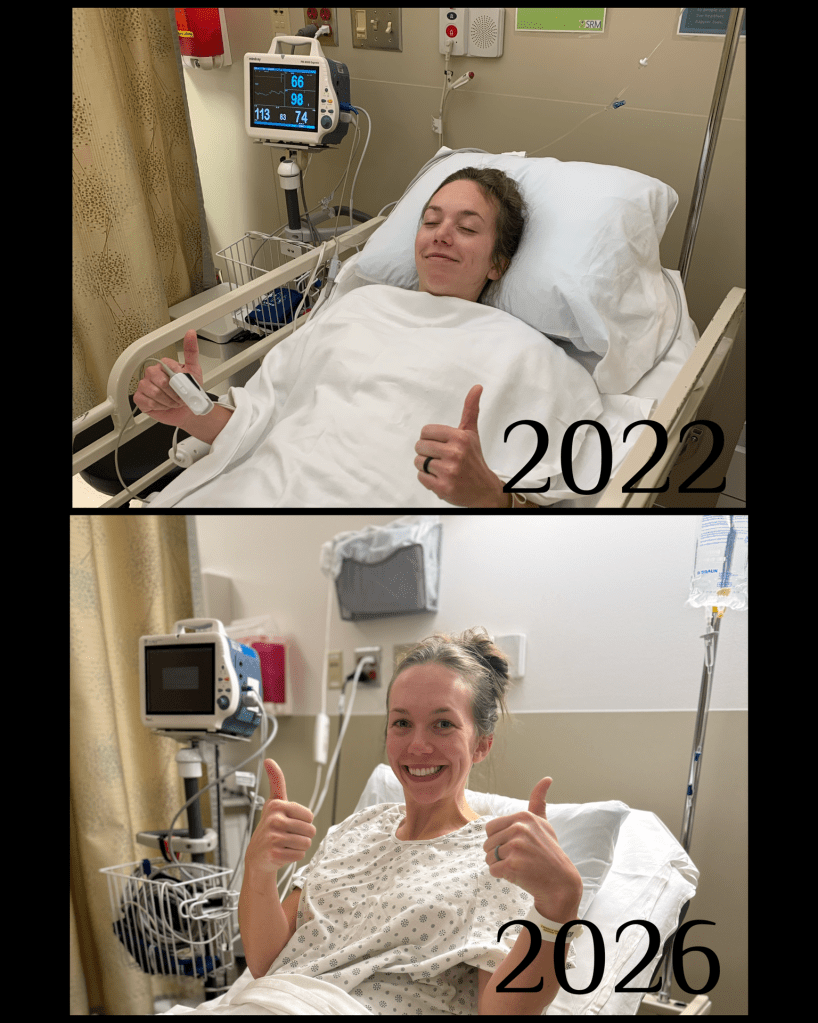
Here we go!